Intrathoracic shunt quantification is a main issue for applicable scientific administration of coronary heart and pulmonary illnesses. Intracardiac shunts quantified by pulmonary to systemic output ratio (Qp/Qs) are typically assessed by Doppler echocardiography, MRI or catheterisation.
Recently, some authors have urged the concomitant use of thoracic bioimpedance (TB) and inert gas rebreathing (IGR) methods for shunt quantification. The objective of this study is to validate the use of this method underneath circumstances the place shunt fraction is straight quantified reminiscent of in sufferers with remoted atrial septal defect (ASD).
This trial is a potential, observational single-centre, non-blinded study of adults seen for percutaneous closure of ASD. Qp/Qs ratio will likely be straight measured by Doppler echocardiography and direct Fick. IGR and TB will likely be used concurrently to measure the cardiac output before and after closure: the ratio of outputs measured by IGR and TB reflecting the shunt fraction.
The major final result would be the comparability of shunt values measured by TB-IGR and Doppler echocardiography.The study has been permitted by an impartial Research Ethics Committee (2017-A03149-44 Fr) and registered as an official scientific trial. The outcomes will likely be printed in a peer-reviewed journal.NCT03437148; Pre-results.
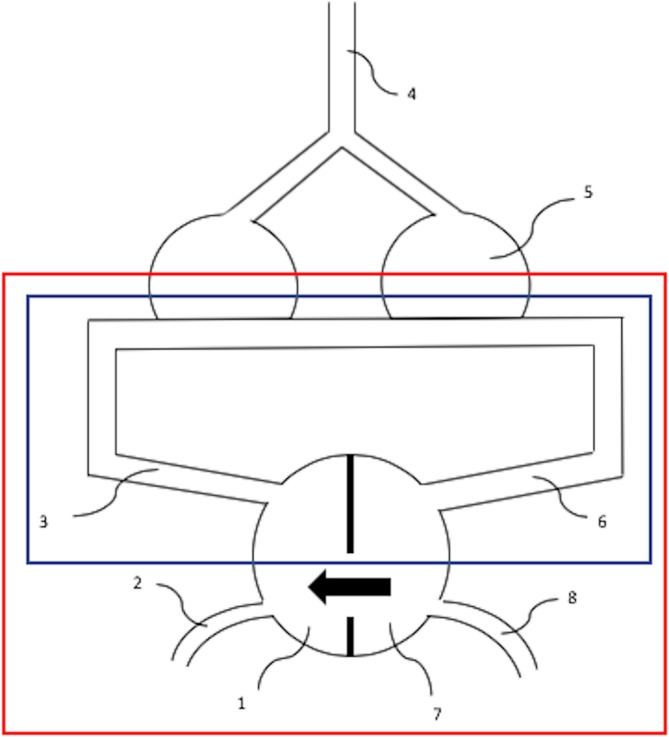
Does the use of an in situ or Y-configuration for bilateral inside thoracic arteries affect long-term survival, patency or repeat revascularization in coronary bypass surgical procedure?
A greatest proof matter was constructed in accordance with a structured protocol. The query addressed was whether or not the configuration of bilateral inside thoracic arteries (BITAs) influences survival, patency or repeat revascularization in sufferers present process coronary artery bypass grafting.
Five hundred and seventy-one papers had been discovered using the reported searches, of which eight represented one of the best proof to reply the scientific query. One systematic evaluate, four randomized trials and three observational research had been chosen. The authors, date, journal, study kind, inhabitants, principal final result measures and outcomes are tabulated.
All four potential randomized trials discovered no important distinction in graft patency or mortality when evaluating Y-graft and in situ configurations. Three of the four randomized trials discovered no distinction in main opposed cardiovascular and cerebrovascular occasions or repeat revascularization at follow-up. An exception was Glineur et al. (Bilateral inside thoracic artery configuration for coronary artery bypass surgical procedure: a potential randomized trial.
Circ Cardiovasc Interv 2016;9:7), who discovered that the Y-configuration resulted in decrease charges of main opposed cardiovascular and cerebrovascular occasions. All three observational research reviewed discovered no alteration in survival, cardiac occasions or repeat revascularization between in situ and Y-graft BITA configurations.
One systematic evaluate discovered related outcomes with respect to mortality, cardiac occasions and repeat revascularization with in situ and composite BITA. In abstract, present literature demonstrates no distinction in scientific outcomes between composite and in situ graft configurations. Furthermore, the configuration of BITA doesn’t have an effect on mortality, graft patency or repeat revascularization.
